Sustainability and data key to the future of the healthcare estate
An overview of the Healthcare Summit, held last week in London

Data collection and sustainability are buzzwords for the healthcare property sector moving forward, according to speakers at this year’s Healthcare Summit, held in London last week.
The event brought together experts from across the public and private healthcare sectors, from investors and developers, to architects, contractors, and product and service suppliers.
As well as an exhibition, there were three conference streams – HealthInvestor, Caring Times Owners’ Club, and, for the first time, Healthcare Property – with speakers providing delegates with information on the challenges and opportunities facing the sector.
In the Healthcare Property stream, chaired by Healthcare Property magazine editor, Jo Makosinski, speakers covered everything from best practice in design and bringing care closer to communities, to the carbon net zero challenge and preparing for PFI contract expiry.

Shoots of light
Harry Hyman, chairman of Primary Health Properties; Emma Glynn, head of healthcare advisory at JLL; and Joe Munro, associate for healthcare at Knight Frank, gave an overview of the property market across acute, primary, private, and social care sectors.
Hyman said there was a demand for new primary care estate, with 50% of existing premises deemed ‘inadequate’, and he estimated the market was worth between £3bn-£5bn moving forward.
However, he also said government reimbursement would be key, adding: “The change of government is fabulous from a healthcare standpoint, but we want to see if the government is long on cash as well as oratory.
“But we need to look at the system for reimbursing rents otherwise there will be no new buildings built in the UK.
“Unless we get the right returns, there will be no new investment.”
Munro added: “It has been a challenging 24 months, but we are seeing transactions going through.
“Funds are looking to really capitalise out of core sectors such as retail and offices into healthcare.”
ESG credentials will play an important role in investor activity moving forward, he added.
Glynn said: “The ‘E’ in ESG is easily measured and reported, but for healthcare the ‘S’ is also very important.
“The social aspect is not just a moral incentive, but an economical one that can ensure long-term viability and care quality and help operators to meet regulatory requirements.
“Some of our investors have turned down transactions due to ESG, leading to better lease terms and lenders offering improved debt terms.”
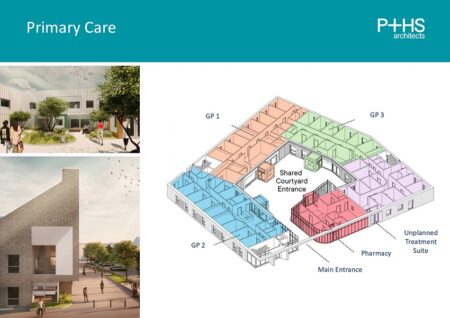
Cath Lake provided an insight into how primary care facilities are being designed with built-in flexibility
Design for life
Cath Lake, director of P+HS Architects; and Paul Yeomans, director of Medical Architecture, also provided delegates with case studies and insight into the design of post-COVID healthcare facilities – with ‘flexibility’ the buzzword.
Lake said: “Even before COVID we have always been trying to design great spaces and a great patient journey.
“But what we are finding is that clients are asking us to design more flexibility into their buildings so they can be more effectively utilised should something like COVID should happen again.”
Examples included a hospital intensive care unit and a new primary care facility designed to bring several GP surgeries together under one roof, and with the flexibility to cope with the possibility of another pandemic.
And Yeomans said this focus on primary care – part of the new Government’s reform of the health service – was leading to a shift in thinking and a number of inspirational developments which are setting a benchmark for the future of more preventative, rather than reactive, care delivery.
Yeomans said: “People have moved on from COVID and it’s about a new world of healthcare – a person-centred preventative approach delivered in the community.
“In terms of our approach to healthcare facility design, this is an important shift in thinking and one we have seen embraced in pioneering community health schemes in recent years, such as The Jean Bishop Integrated Care Centre in Hull.
“It’s about long-term investment in the right community-focused facilities and bringing savings to the wider system.
“It sets a new standard for community health facilities and we are hopeful these initiatives demonstrate benefits so we get the long-term investment we need moving forward.
“From small acorns come bigger things.”
Melissa Magee said operators were increasingly retrofitting and extending existing building rather than construction new facilities
Economic pressures
Melissa Magee, managing director and architect at Carless + Adams, focused her talk on social care design, where there has been a move away from large care homes to cluster-style household models which offer more independence.
And she said the current economic pressures had meant operators were shifting towards refurbishment rather than new-build developments.
“It’s about bespoke designs which fit with operators’ needs, their residents’ requirements, health and safety legislation and regulatory demands, topography, landscaping, neighbourhood, and integration – where residents’ needs can be fully catered for.
“We are being asked to design spaces with identifiable areas to reflect the makeup of societies and which are designed with a knowledge of the area in mind, not just adapted to suit.
“We are past the point of institutional and clinically-led buildings.
“And buildings must be flexible. If there’s one thing COVID has taught us it is that one size does not fit all.”
Opening the front door
The Government’s pledge to reopen the front door to the NHS through improved primary care services was also the talking point of a session entitled ‘Lift and Shift – Health on the High Street’.
This looked at how changes to planning policy are making it easier for healthcare operators to repurpose high street buildings – such as empty department stores and offices – as community-centred medical and wellbeing facilities.
Andrew Ryley, director of planning at DLBP Planning Consultants, said: “We have a positive and permissive planning environment for health and healthcare-related developments – if you can demonstrate need.”
Guy Kippen, associate development director at Prime Plc, added: “Health on the high street makes perfect sense.
“The cost of development at the moment, and how we think about health services, as well as changes in the retail market, means healthcare is seen as a good investment.
“In turn, locating health services in the high street increases footfall and gives economic certainty.
“It is also better for the environment to be utilising existing buildings.”
But he added that these high street developments worked best when they involved more than just healthcare professionals – providing facilities for everything from social care and local authority services to emergency services, pharmacies, and charity organisations, all under one roof.
“NHS systems and processes are not the quickest and to really achieve the best spaces we need a different approach,” he added.
“Where it has been done well it has been led by one of the partners.
“You need a whole-system buy-in and support needs to come from the top tables in all organisations.”
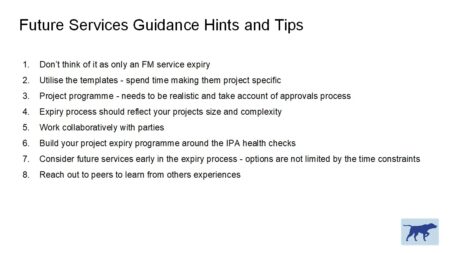
Speakers looked at how operators can approach PFI contract expiry
Life after PFI
Speakers also provided an overview of how healthcare operators can address the issues surrounding the expiry of PFI contracts.
PFI was introduced by John Major’s Conservative government and meant the upfront cost of building public facilities such as hospitals and schools was taken on by the private sector in return for repayments to cover construction and maintenance, typically over a 25-year period.
These contracts are now heading towards expiry, and this could mean trusts find themselves faced with having to take over management of the facilities, potentially lose buildings, or be hit with high-cost break clauses.
The Infrastructure and Projects Authority (IPA) recommends beginning to prepare for contract expiry seven years prior to handback.
Alison Martin, partner at DAC Beachcroft said: “PFI, like it or not, was a key model for the delivery of critical infrastructure in the NHS and manging expiry and transition is a really-important part of trusts’ financial planning going forward.
“The overarching message is preparation, preparation, preparation.
“We need to ensure all the PFI documentation is there – all the schedules and any amendments, additions, or updates.
“It is also critical to know what the contract says about handback and expiry.
“If there is going to be a dispute, it will come down to what the contract says and in some contracts we have seen the provisions are quite vague and trusts will need to review and assess the clarity and practicality of some of these.
“We know not all assets will transfer back to the trusts on expiry. Some might stay with the private sector and understanding that is key for future provision.
“We also need to ensure we know what condition the estate is in.”
Jack Banks, a partner at P2G Contract Support, added: “It’s about how we ensure disputes are handled and everyone has an outcome that suits them.
“Project resets will create a safe space to mitigate some of the issues and to work out what does and doesn’t need to be done so there is absolutely clarity on what should be delivered in the remainder of the contract.”
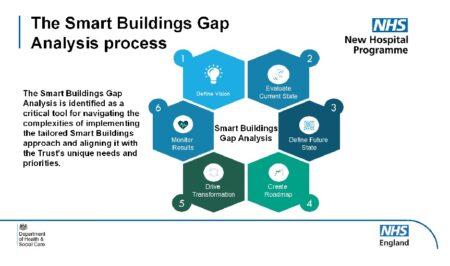
Creating SMART buildings is critical to the future of the estate
Looking to the future
On what funding model might come next to replace PFI, speakers hinted it would likely continue to involve the private sector.
Martin said: “We have not got a clear idea of what future models will look like, or what role the private sector will continue to play, but when PFI contracts come to a hard stop private sector involvement in the delivery of healthcare infrastructure isn’t going to cease completely otherwise the NHS will not have the capital needed to deliver improvements and we will return to decrepit estate we had before.
“The Government has hinted it will use private finance in the delivery of the NHS estate going forward, and there will probably be a mix between private and NHS capital.
“There also remains significant questions over whether the private sector will want to get involved going forwards.”
Banks added: “The jury is still out on whether the market can demonstrate good use of funds and if PFI maintenance models were good value for money.
“Have the hospitals that were built 20 years ago been maintained and are they in a better condition now than they would have been if procured through traditional routes?
“We are seeing some contracts being extended because they can’t clear the programme of works needed to bring them up to standard.
“There are models emerging in Scotland and Wales and it’s about what is the key model for capital growth. Is it private finance or looking at the way services are received and delivered?
“Any future model will have to draw on the successes of PFI, of which there are many.”
Data is king
Also speaking on PFI was Olú Aláká, director of estates and facilities at University College London Hospitals NHS Foundation Trust, which has 15 years left on its PFI contract, but is already working on the handover process.
He said: “In 15 years this 17-storey building right in the heart of London, with all its complexities, is going to get handed over to me and my team and I will have to manage it.
“At the moment the PFI provider is doing it and our role is to performance manage them in line with the contract.
“We have two options. We can either continue as we are and come handback everything is reactive; or we can learn from the PFI and take a preventative maintenance approach.
“That’s the journey for us between now and handback.
“And the key will be data.
“Data is king and whoever has the data is king.
“The first thing we are doing is understanding the data so there is one single version of the truth so that when it comes to handback it’s easier.”
The importance of data was also the theme of a talk on SMART hospitals, headed by Karl Redmond, strategic estates lead in the NHS Estates Delivery Unit.
He revealed that many trusts had signed contracts with IT suppliers which meant they had to pay for any data held about their estates.
He told delegates: “Hospitals are not just about bricks and mortar, they are also about data and we are trying to make sure we optimise our healthcare estate.
“The development stage of a building is 0-5 years, but the operational stage is 30-60 years, so we need to have SMART buildings, and not just SMART buildings, but intelligent buildings.
“People say if you’re doing BIM, you’re doing SMART buildings, but they are two different things
“Estates are already failing because operational teams do not know how to access and use the data.
“If we do not do something different, we will end up with the same outcomes and it’s not working.
“We want to own our data and for it be free of charge. It’s my data and I shouldn’t have to pay for it!”

The carbon challenge
The day ended with a presentation on the health sector’s carbon net zero challenge, with speakers Adam Mactavish, group sustainability director at Currie & Brown; and Rob Walton, partner at RWK Goodman.
Again, they said data was critical to understanding both where the sector is currently at on its journey, and how it can get to the finish line.
Mactavish said: “The New Hospital Programme will only deliver 10% of the energy savings we need, so it’s about how we go about the other 90%, and the vast majority of that won’t be in new hospitals.
“We need to make better use of the estate we already have.
“Hospitals are the most-energy-intensive buildings outside of data centres and trying to change systems like ventilation, heating, and cooling is very complex, but that’s the challenge we face.”
He said hospitals were having to decommission Combined Heat and Power (CHP) plants as these run on gas and replace them with electric alternatives.
However, with electric systems, running costs are often higher.
“A first step is drilling down into the data as there is currently a lack of detailed information on how buildings are being controlled.
“We need to use data to understand lifecycle expenditure and how we can have a better-performing estate.”
Join us next year
Commenting on the summit, delegate, Arjun Sharma of Oakridge Care, said: “The discussions around the integration of technology were truly eye-opening.
“I left the Healthcare Summit feeling inspired and equipped with new ideas to implement in our care home.”
Sarah Wheeler of Capsticks Solicitors added: “It was great to hear about market trends and investment opportunities while catching up with new and existing contacts.”
And Steve Fergus of Barclays said: “I was seriously impressed by the breadth of content and presenters that was on show at the summit – the hardest decision was working out which sessions to attend and which ones to miss!”
To find out how to join us at next year’s event, click here.
